Officials from several Oklahoma hospitals gathered in Oklahoma City Tuesday to strike an urgent tone in their pleas with Oklahomans to wear masks, get vaccinated and keep the state's health care system from collapsing in on itself as the rates of COVID-19 infections, hospitalizations and deaths appear poised to eclipse previous surge records.
"The reality is that hospitals have limited resources – staffing, beds, and supplies are all limited," said Dr. Bahar Malakouti, a neurohospitalist and medical director for stroke at Mercy Hospital Oklahoma City, https://vimeo.com/588400896">at a press conference Tuesday on the grounds of OU Medical Center. "When we have the kind of increase in COVID patients that we’ve seen here in Oklahoma over the last month, all our resources are stretched beyond our limits. Our staff is burned out and wondering how we’ll survive yet another surge."
"I’m here to tell you the current level of community spread impacts every single Oklahoman," Malakouti said. "This most recent surge in COVID has had a dramatic impact on nearly every health care service our hospitals provide. If you get in a car accident, have a heart attack, need an emergency surgery or, yes, even if you have a stroke, there’s a chance you might not be able to get the time-sensitive care you need."
Malakouti noted that on many days over the last month, there has not been a single bed available at many Oklahoma hospitals. She said in some cases patients in the Mercy system are being transferred to hospitals in Kansas, Texas and Colorado because there are no available beds in any Oklahoma hospitals.
"And this is currently a physical bed issue at Mercy, not a staffed bed issue. We are routinely running out of physical beds to care for all patients – both COVID and non-COVID - who need us," Malakouti said.
SSM St. Anthony Medical Center registered nurse Regan Wickwire said she had been working the hospital's COVID ICU since the beginning of the pandemic last spring.
"Not only are patients flooding into area hospitals at a rate higher than at this point last year, but the patients are sicker," Wickwire said. "And they are much younger. We are seeing critical COVID patients in their 20s, 30s and 40s this time around, with a lot of life left to live. They are scared. When they reach our unit, they very much believe the virus is real."
"I can't tell you how many patients I've sat next to, stroked their faces and let them know they are loved and appreciated" as they died, Wickwire said, noting many of their last words with loved ones happened via FaceTime calls.
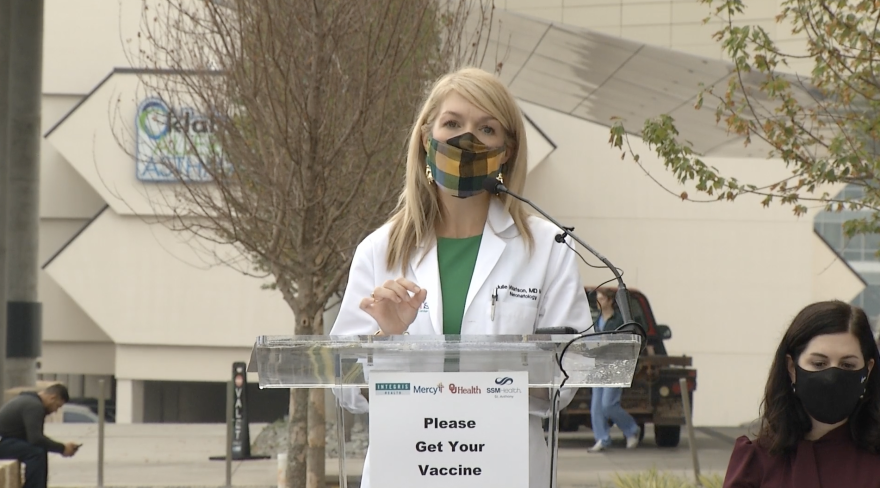
Dr. Julie Watson, chief medical officer at INTEGRIS Health, said she knows Oklahomans are weary.
"The best solution we have right now is the vaccine," Watson said. "And yes, even though some vaccinated people are testing positive for COVID, the risk is 600 times less likely that they will need the hospital to get better compared to those who are unvaccinated.
"In fact, more than 90% of all patients who come to us hoping that we can save them, help them breathe again, stop their kidneys from failing from COVID, haven't taken the vaccine. 93% of Oklahomans who have been hospitalized in the last month with COVID have not had the vaccine. These patients believe in us when they are sick, but seemingly haven't trusted us when we've shared with them how to stay well. It is heartbreaking and exhausting," Watson said.
"Please get vaccinated. Don't put yourself, your family, your children, your neighbors at risk. Please don't wait until you are lying in a hospital bed. Vaccines don't work at that point. Please get your vaccine so we have beds to care for patients with cancer or diabetes or heart disease. Get it now. Get it today," Watson said.
“Our healthcare providers simply cannot keep going at the current pace,” said OU Health chief quality officer Dr. Dale Bratzler.
OU Health noted in a statement that, "The number of new COVID-19 infections has risen dramatically in Oklahoma. In the past week, there have been 15,490 new infections reported in Oklahoma, which is an increase of 10% over last week. One thousand three hundred and ninety two (1,392) people with COVID-19 are currently hospitalized in Oklahoma, and 369 are in the ICU. There have been 131 deaths because of COVID-19 in the past week."
"The majority of infections are caused by the Delta variant, which is much more contagious than past versions of COVID-19. Because Oklahoma’s overall vaccination rate remains below 50% and mask-wearing has decreased significantly, the Delta variant has been able to spread rapidly," Bratzler said.
"You have to think that any person you encounter could be infected. There is no way externally to know. A person who is infected with Delta variant may be asymptomatic or have minimal symptoms and infect you," Bratzler said.
In a separate press conference in Tulsa on Monday, officials from Saint Francis Health System shared similar dispatches from their hospitals and clinics, noting patients are being treated in hallways and waiting rooms, and in some cases having to be admitted for care in chairs rather than beds.
"Last week, we had a woman in her 30s who was 38 weeks pregnant and we could not save her or her unborn child," said Dr. Ryan Parker, chief of emergency medicine at Saint Francis Hospital. "We had a 40-year-old man that passed away over the weekend. And I think that you guys are all seeing this play our in the nationwide media, but, for us, these are our brothers and our fathers and our children and our uncles, and so it is very personal for me when we lose these patients."
Parker said the average age for COVID patients requiring mechanical ventilation is now 51, far younger than during the last surge before the widespread availability of vaccines.
Cliff Robertson, Saint Francis Health System CEO and president, said he supported mask mandates both locally and for the state, given masks' proven efficacy in reducing the spread of COVID-19.
"We are supportive of mask mandates if the city council deems that appropriate for Tulsa, or at the state level we would be supportive of those, as well," Robertson said.
Parker said masks in schools are crucial to protect children.
"I think that it's our jobs as parents and citizens to protect our kiddos, and we know that the kiddos aren't able to be vaccinated until they're 12 as of right now," Parker said. "To protect those kids, and especially to protect them from mitigating and spreading the virus to their teachers, their grandparents, their parents, that mask is another level of protection."
Oklahoma State Department of Health Commissioner Dr. Lance Frye said Friday he would not comment on whether K-12 schools should require masks, as is recommended by the American Academy of Pediatrics and the federal Centers for Disease Control and Prevention. Under a law signed by Gov. Kevin Stitt in May, public school districts in the state are legally prohibited from requiring masks, though two districts in Oklahoma City have implemented pseudo-mandates with opportunities for parents to opt their students out. The governor last week issued a statement in support of those policies, saying they respect parents' choice to send their children to school without masks.
Stitt has not held a press conference to address COVID-19 or its impact on Oklahomans since March 29.